Dr. Robert Louis, a neurosurgeon at Hoag Memorial Hospital Presbyterian in Orange County, CA, is pitched some type of new technology, gadget or medication every day. He’s shown things so often that he developed an internal filter that automatically sets expectations a lot lower than the enthusiasm of the rep. But that all changed in October 2015.
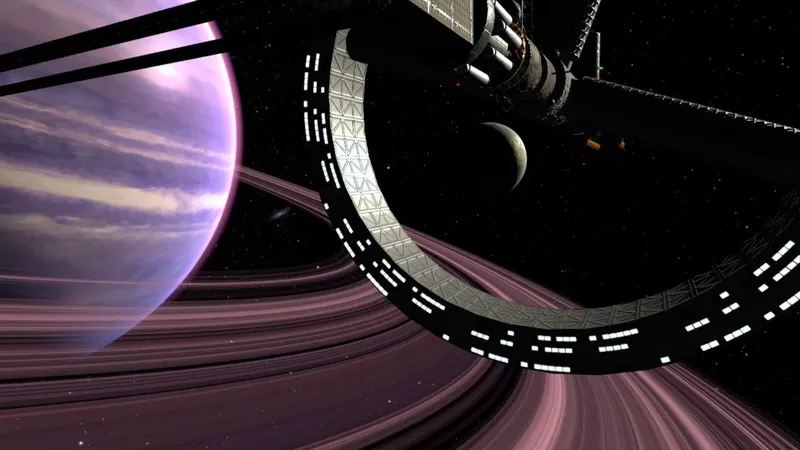
That’s when Surgical Theater reps dropped by to showcase the Surgical Navigation Advanced Platform, or SNAP. Designed by former Israeli fighter pilots, the technology uses virtual reality to allow neurosurgeons to “fly” through a patient’s brain to get a better look at tumors, nerves, blood vessels and tissue prior to surgery. Before surgery, the patient’s brain is captured and recreated as a 3D model for Dr. Louis or his colleague Dr. Christopher Duma, neurosurgeon and director of Hoag’s Brain Tumor Program, to navigate.
Hoag is currently using an Oculus DK2, but the FDA recently cleared the consumer Oculus Rift for use and that will be deployed moving forward in all medical facilities, according to Jim Breidenstein, president and COO at Surgical Theater’s SNAP division.
http://youtu.be/t2qO015yAl8
Louis said prior to the introduction of this technology, he’d have to reference black-and-white 2D “slices” of the brain and then use his imagination (and 20 years of surgical experience) to map out the surgical procedure in his head before entering the Operating Room.
Since SNAP is registered with both Stealth, a technology Hoag uses, and Brainlab, that 3D model of the patient’s brain is used to track the tips of the instruments as the neurosurgeon navigates the brain. It works like a GPS inside the head, allowing doctors to track their instrument in real-time.
“Instead of looking at a 2D model, I can now see the tips of the instruments on the 3D Surgical Theater System on screen and compare that to what I’m seeing through the lens of the microscope,” said Louis, who is also director of Hoag’s Skull Base and Pituitary Tumor Program.
Hoag, one of 10 hospitals using this technology, has already used SNAP on 100 patients.
“We’ve seen an increase in the rate of complete tumor removal and a decrease in the rate of neurological complications,” Louis said.
Louis said this new technology helped him save Marcus Barnes, 41, who had a brain tumor. Louis focuses on non-evasive surgeries whenever possible, preferring to take tumors out through the nose, ear or eyebrow whenever possible. His original plan was to make a small incision by the eyebrow for Barnes, but when he put on the Oculus headset and explored the virtual reality model of his brain, he found that the patient’s optic nerve would block him from extricating the entire tumor that route.
https://youtu.be/F8v7vSxBTmQ
“We changed the approach and we did a small incision behind the hairline instead,” Louis said. “We made this change before even touching the patient and we were able to get the entire tumor out successfully.”
SNAP also played another role in this particular operation. The technology has been designed so anyone, including patients, can get a look inside their head. Louis wheeled the headset into Barnes’ room while he was being prepped for surgery so he could show him why he was changing the operation the morning of, which Louis admits is something that would normally make a patient nervous. But this technology allowed the patient to see exactly what the doctor sees – and will see during surgery.
“Everybody loves seeing their brain in 3D and in color,” Louis said. “They feel much more engaged in their own process with VR. It goes from ‘I trust you’ to ‘I understand what’s going on with my body.’ Research shows patients who are more engaged and have a better understanding of their pathology will have a better outcome.”
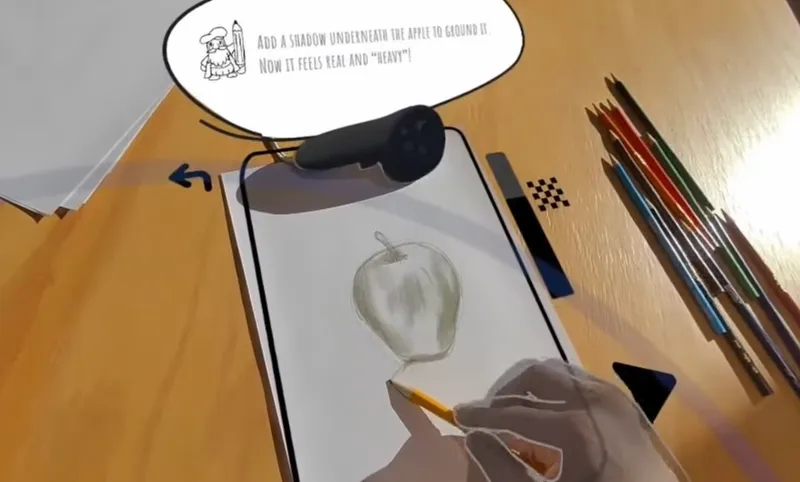
In September, Louis will begin testing a brand new augmented reality technology from Surgical Theater. The new technology will be used inside the OR, and use the 3D model of the patient’s head to project a real-time 20-30% shadowed view of exactly where the tumor is via AR while the neurosurgeon is performing the operation through the lens of a microscope or viewing the screen of the endoscope.
“The tumor is visible partially in my field-of-view so I know exactly what direction I’m going,” Louis said. “I don’t think AR will replace the pre-op rehearsal in VR, but it adds to the tools we use during surgery and it’s another big advance to be more precise.”
Louis said the less disruption of normal tissue and critical anatomy in getting to the tumor, the fewer neurological complications and less blood loss there is for the patient.
There are 10 hospitals using this VR technology today, including University Hospitals Case Medical Center, University Hospitals Rainbow Babies and Children’s Hospital, The Ronald Reagan UCLA Medical Center, The Mount Sinai Hospital, Mayo Clinic and NYU Langone Medical Center. Some of these hospitals are using SNAP in an additional way.
VR can also be used to train residents, Breidenstein said.
“Students can see in 20 minutes what has taken neurosurgeons like Dr. Louis 20 years to perfect in his own mind,” Breidenstein said. “It can dramatically shorten the learning curve of tomorrow’s surgeons.”
At UCLA, Dr. Neil Martin uses Surgical Theater to travel pre-operatively through a patent’s head.
There are multi-user options, so the doctor and the student each can have an individual avatar and they can look at the anatomy of the brain from a teaching perspective. This option is also available online, so that the doctor and student don’t have to be in the same state or country.
Breidenstein said over 2,000 patients have been treated using Surgical Theater technology to date.
“By design, we’ve had a limited launch and strategic plan with 10 centers for the current physical year,” Breidenstein said. “In 2017, we’ll take our technology and expand and scale it based on the learning and volumes of clinical data we’re collecting. Our goal it to get SNAP into all key centers in the surgical world.”
Alon Geri, co-founder and executive vice president of engineering at Surgical Theater, said SNAP has been designed to evolve with technology. The Windows-based technology already works on both Oculus Rift and HTC Vive, as well as several enterprise AR devices. Geri said any headset that will be available in the market will be supported in the future, when it makes sense.
Geri, who used to fly Blackhawks in the Israeli Air Force, ended up designing this virtual reality technology on a challenge. He had spent several years developing a virtual reality flight simulator for pilots when a neurosurgeon asked him if he could do the same thing for doctors. He accepted the challenge.
“Once surgeons started to experience it, it blew their minds,” Geri said. “It allows them to prepare for complicated surgery cases and gets them into the zone to go under the microscope.”
Louis said using SNAP “is a no-brainer.”
John Gaudiosi is a freelance reporter with experience covering the world of videos game for multiple outlets, such as Fortune and [a]listdaily. Follow him on Twitter: @JohnGaudiosi.